What is End-of-life Care?
End-of-life care is care provided in the days, weeks or months before an individual passes away, supporting emotional and spiritual support, physical comfort and practical tasks. The last year of life is referred to as “end-of-life care”.
End-of-life care is regularly provided by clinicians, carers, nurses, family members, physicians, and other support workers at home, in a long-term care facility, or a hospital. Moreover, facilities may have palliative or hospice care specialists offering end-of-life care services.
We all deeply value living as fully as we can until we die. In the final months or the last year of life, personalised care for a loved one results in a better experience tailored to their needs and wishes and more qualified health and care services. Community nurses usually visit the patient at home, and relatives and friends may be closely involved in caring for them.
How Long is End-of-life Care?
End-of-life care is approached when a patient is likely to pass within a year, although no one can predict death. This kind of care should begin when you need it, whether it lasts for a few days or months.
Guidelines for the care of people who are dying in their final days of life have been released by the National Institute for Health and Care Excellence (NICE). This manual addresses common symptom management and treats the dying individual, their loved ones, and carers with decency and respect.
The Fundamental Principles of End-of-life Care
There are fundamental principles of end-of-life care that include:
- Empathetic communication
Empathetic communication ensures that the person and family understand what is going on and that previous care plans have been discussed. Specialists should communicate significant changes in the individual’s condition to the relatives. If death conversations have not yet taken place, families must prioritise them.
- Comfort and dignity
Even though there may be indications that the patient is dying, the treatment professional providing end-of-life care must make the diagnosis. The main focus of care should be on preserving comfort and dignity during the final stages of life.
- A holistic approach to care
A continuous review of the needs and symptoms of the person using a holistic approach will enable an improved view of the person’s spiritual, emotional, physical and social needs.
- Family and loved ones support
At this stage, the support of family and relatives is exceptionally important. The repercussions can be extensive if family members are not supported, or the person does not have a “good death.” In England, there is specific guidance for the last days of life, resources and support which aim to find respectful conversations to improve end-of-life care. This guidance directly involves the dying person and the family member vital for making decisions regarding his passing away.

Conditions That Require End-of-life Care Services
End-of-life care includes individuals near the end of their life from:
- A life-limiting illness, such as a stroke
- A terminal illness, like cancer, motor neurone disease, and dementia.
- A life-threatening acute condition such as an accident
- A sudden crisis in the existing condition
Support an End-of-Life Care Patient Needs
Depending on the patient’s needs, different health and social care professionals may be involved in end-of-life care services.
The carer should support the person to be as comfortable as possible until they die, especially:
- physical needs, including pain relief and management of other symptoms
- emotional needs, including managing distress
- relationships with others, including who they would and wouldn’t like to be with them
- environmental needs, such as their surroundings and community
- cultural, spiritual or religious beliefs and practices
End-of-Life Care Plan
End-of-life planning entails considering and discussing your wishes for medical treatment throughout the final months of life. This can involve receiving procedures that the patient may not desire.
By making plans in advance, the patient can talk about their desires and feelings with their family and friends while they still can do so. Why plan ahead? When the family must make choices regarding care, it can be valuable to let them know your health and social care wishes and decisions.
For every dying person, ongoing pain assessment and management are crucial.
Planning for End-of-Life Care
Focusing efforts on showing care and compassion when carers, family members, and loved ones are aware of the patient’s treatment wishes later stage in life are vital. It is necessary that anyone who has been diagnosed with a life-limiting illness share their feelings with their loved ones before a medical emergency occurs in order to ensure that everyone in your family is aware of the patient’s wishes approaching the end. This is sometimes called advance care planning.
- Get prepared early
If discussions regarding accommodation, treatment, and end-of-life choices are held as early as practical, the path to the end of life is significantly more straightforward. Before they are necessary, consider spiritual practises, memorial customs, and hospice and palliative care services.
- Put values first
Act based on what you feel or know to be your loved one’s wishes if they haven’t made a living will while they are still alive. Create a list of the discussions and moments that best represent their beliefs. Think as much as you can about the patient’s perception when making decisions concerning their care, environment, and passing away.
- Legal advice and financial guidance
Consult legal advice and get financial guidance while your loved one is still alive. Legal documents can state a patient’s preferences for future medical treatment like a living testament, power of attourney, or living will so that all members of the family are aware of their decisions.
- Be in communication with your family
Choose one family member that will be the decision-maker to manage the communication, support and involvement. To support or be against life-prolonging treatment requires clear communication, even while families are aware of their loved one’s desires.
- Settling family disputes
Family conflicts are usually brought on by the stress and grief brought on by a loved one’s illness. Contact a professional physician, carer, or hospice professional to mediate if you and a member are working to come to an agreement on housing arrangements, medical care and support, or end-of-life requests.
- If there are children in the family, consider including them
Children require open communication about their loved one’s health and any changes they notice in you that are age-appropriate and honest. They might find it helpful to express their thoughts through artwork or puppetry, or conversations that explain events in a way they can understand because they may be profoundly impacted by events they do not understand fully.
Although each patient’s and family’s needs are unique, most patients prefer to spend their final days following their death at home, where they may live as comfortably as possible and be close to their loved ones. Transitions can often be challenging for terminal illness patients, especially one who has severe Alzheimer’s disease or another form of dementia. Before they reach the final stage of their illness, patients find it easier to adapt to a new home or care facility. Planning is essential in these circumstances.
End-of-Life Care Pathway
It can be emotional to bring up death discussions with a loved one. For the same reason, it can be challenging for social care professionals to discuss an end-of-life plan with a dying or seriously ill person’s family.
The End-of-Life care pathway is a plan that details the tasks that various professionals must carry out as patients approach the end of their life. Medical professionals must complete some actions to ensure the patients of their physical and mental health in a way as comfortable as possible. It can be sensitive to bring up death discussions with a loved one.
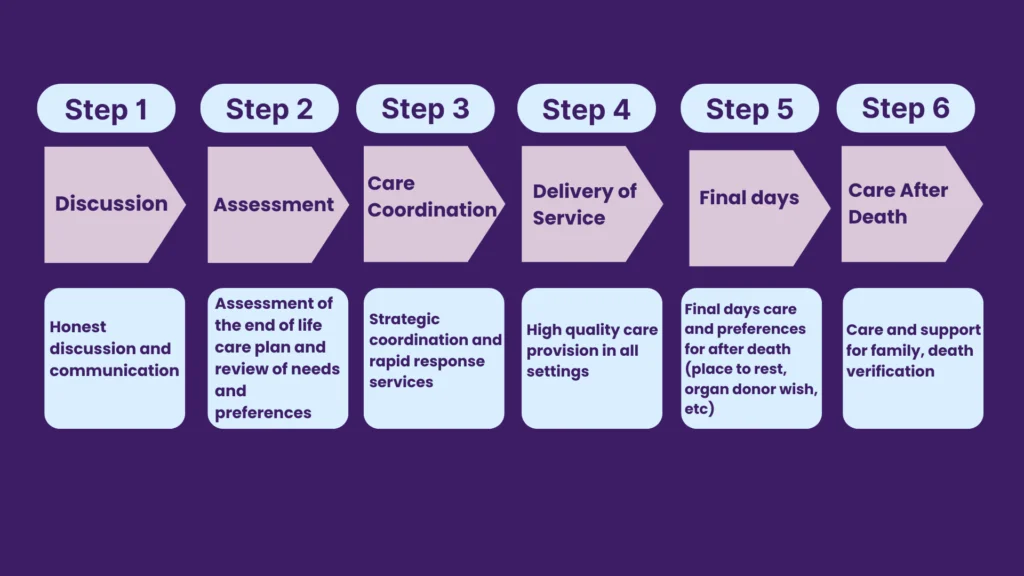
An end-of-life pathway can be developed and implemented in 6 steps. Here is an overview of what you should complete if you are involved:
Step 1 Discussion – Discuss how to deal with a person’s death. The patient is about to pass away; therefore, you need to speak with them, their family and friends so that everyone is aware of the situation and decide who will be making decisions.
Step 2 Assessment – Understand the medical wishes and needs of the patient. Be mindful of dietary restrictions, home care preferences, and other cultural or religious needs.
Step 3 Care Coordination – Each patient will require different care and guidance. Plan to have a qualified team of professionals on-site who are prepared to manage the needs, such as nurses, nursing assistants, healthcare professionals, carers and doctors.
Step 4 Delivery of Service – The plan is implemented at this point. Care must be provided in the safest environments and in agreement with the patient’s needs whenever possible, always ensuring consent.
Step 5 Final days – Knowing what death looks like will help you prepare for it. You may make the final days of a dying person comfortable rather than distressing, by being aware of what to expect.
Step 6 Care After Death – It is extremely important to carry out funeral arrangements and support the patient’s family in making decisions after death.
Palliative Care and End-of-life Care
Palliative and end of life care affects everybody across the lifespan, however more people are expected to die at an older age, allowing us to plan and consider their wishes and choices for their end-of-life treatment.
NHS released statistics from the Office of National Statistics (ONS) on registered death cases in 2017. This shows that 78% were people aged 70 or above, and 22% were aged 90 years or above. Death and grief affect every aspect of people’s lives. These health and social care events are strongly tied to end-of-life and palliative care.
Palliative Care
According to the WHO (World Health Organisation), palliative care enhances the quality of life for patients (adults and children) and their families dealing with issues brought on by a life-limiting illness generally progressing. Early diagnosis, accurate assessment, and treatment of pain and other psychological, physical, or mental health issues prevent and decrease suffering.
Many healthcare professionals, such as community nurses or general practitioners, may provide palliative care to individuals as part of their job. For an additional palliative care specialist, palliative care nurses or counsellors trained in this type of care can provide a service to individuals and families in need. The team of healthcare professionals specialising in palliative care can coordinate the care of patients with terminal illnesses.
Difference Between Palliative Care and End-of-life Care
Palliative care is available the moment you learn you have a terminal illness. You may receive palliative care and the usual treatments for your condition. When you’re approaching the end of your life, you will receive end-of-life care, a type of palliative care.
These are the differences between palliative care and end-of-life care:
- End-of-life care is for those in their final weeks or months of life, while palliative care is for anyone living with a severe illness at any stage, including the day when first diagnosed.
- Palliative care is received by patients coping with pain, distressing symptoms, and severe side effects caused by a terminal illness or the treatments received meant to cure it. In comparison, end-of-life care is provided to patients with six months prognosis or less.
- A consultation for palliative care can be offered at your home, in the outpatient clinic, at a specific hospital, and in your community. Home care, nursing homes, assisted living facilities, and inpatient hospice facilities all offer end-of-life care.
- Palliative care is for individuals who want curative care, while end-of-life care is for those who have chosen to renounce it and prefer comfort care in their final months, weeks, or days of life.
- A board-certified palliative care physician, nurse, social worker, and healthcare coordinator offer this service. A Board-Certified Specialist, Nurse, Social Worker, Spiritual Support Counsellor, Certified Home Nurse, and Volunteers provide hospice care.

Why is End-of-Life Care so Important
End-of-life or hospice care provides support, comfort and quality of life by relieving pain and reducing feelings of despair. Carers managing and delivering services think of their practical and emotional needs and the support they can provide to adults approaching the end of their life.
According to the National Audit of Care at the End of Life, 82% of people who were close to the dying person felt supported by the carers after the person passed away. End-of-life care, also called hospice care, includes help managing the dying person’s emotional and mental distress. It is vital to treat emotional pain and anxious feelings.
The carers try to provide gentle physical contact and can help lessen the pain through slow communication by asking them what they need.
End-of-Life Care Options with Unique Community Services
At Unique Community Services, the quality of people’s end-of-life journey is key to our humanised care ethos. Our clinicians offer empathetic support that reflects as much comfort as possible to people, bringing more compassion during the last months or days of their lives. They assist with administering medications and provide measures for the relief of symptoms. Our heart-led approach gives comfort and understanding to the patients and their families.
Our competent clinicians, as healthcare professionals, will support and care for your loved ones by building trust as the journey progresses. Being present and listening attentively is our fundamental, because we understand how the presence of clinicians can be the greatest gift to families and their loved ones.
You can contact our offices in Bristol and Manchester or us directly here on our web page. Our expert team is ready to give you the required information.
Please get in touch with us. We are ready to support you!